New viruses in the coronavirus family often originate in animals and are then spread to humans, but how does knowing this help doctors and scientists to track and treat the latest outbreak?
What happens when there is a new disease?
The first case of any new bug is usually spotted by a health professional noticing a pattern or cluster. For example, a doctor seeing many patients in a short period with the same symptoms, particularly if patients are becoming seriously ill and when tests for known pathogens come back negative.
A doctor suspecting they are looking at an outbreak of a novel virus or bacterial infection would contact their local health department who would arrange for samples from the affected patients to be sent to a research laboratory for investigation.
History is key to the mystery
A very important role of doctors seeing these patients is to take a thorough history. This involves asking about more than the patient’s current symptoms; doctors need to know when and how symptoms developed, where the patient has been, what they have been doing, who they have had contact with and how quickly they became ill after exposure to any possible sources of infection.
This information is important for pathology testing to know what tests are appropriate to rule out known viruses or bacteria, but also for a research laboratory to know what sort of infection they might be dealing with.
Dr Lyn Waring is a microbiologist based in Melbourne, she explained;
“One of the beauties of bacterial cultures is that they grow, you can find what’s there. There are some exceptions however, such as legionella which doesn’t grow on commonly used agar plates, so in a pathology laboratory you need to have a lot of knowledge to understand what you might be missing.
One of the limitations of molecular testing is that it only finds what you’re looking for, so viruses can be difficult to detect. Many viruses are self-limiting so patients won’t get seriously ill, but with outbreaks such as this latest one we need to be able to diagnose it.”
The first cases of the new coronavirus are thought to have come from a seafood market where there were also live and newly slaughtered animals. Knowing the symptoms combined with the patients’ attendance at the market where animals were present, would have helped scientists narrow the field to a suspected coronavirus when they first began sequencing of the viral genome.
Dr Waring said; “With the new molecular methods, once you figure out what group it’s likely to be, based on the history, you can start sequencing to get the virus’ genetic code.”
Although there may not be a specific treatment for this new coronavirus yet, a patient who contracts it will have a higher risk of secondary infections, which is why it is important for doctors to know when someone has the virus so they can provide supportive care and manage any secondary infections.
Communication and cooperation
In Australia, every state health department has a reference laboratory and these share information with one another as well as with international reference laboratories to keep a log of existing pathogens that is updated as new ones are discovered.
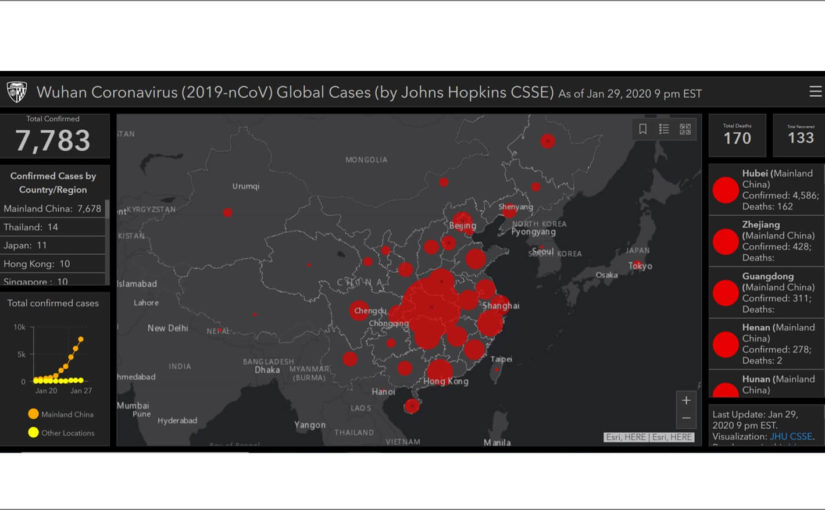
Once scientists have sequenced a virus’ genetic code, they can then begin to develop a test assay for it, to diagnose anyone suspected of having the virus and track its spread in the community.
A combination of pathology test results and comprehensive patient histories is what allows health professionals to understand the virus better; who is being affected and how it is being spread. They can then develop a case definition which helps doctors identify those most at risk, consider quarantine, and prioritise these people for testing.
Pathologists are trend-spotters
Pathology laboratories see trends more quickly than they might be seen by other health professionals operating in the community, because the lab receives samples from multiple referring doctors so they see more confirmed cases of a disease than individual doctors would. Pathology laboratories work closely with the health department to report notifiable diseases and unusual outbreaks.
As the word spreads pathology also has an important role in triaging cases. Dr Waring said; “We see a flurry of activity as people hear more about an outbreak in the media. Understandably people get worried, but this can choke up the system.
Pathology is all about doing things in a logical, orderly fashion. We deal with urgent cases all the time, we have to be good at prioritising to deal with the most urgent cases first.”
This collaboration between treating doctors, pathology teams and health departments is what helps protect the community in the event of a disease outbreak.
*Image: John Hopkins CSSE coronavirus map
The latest situation reports on COVID-19 with figures from the World Health Organisation are also available here