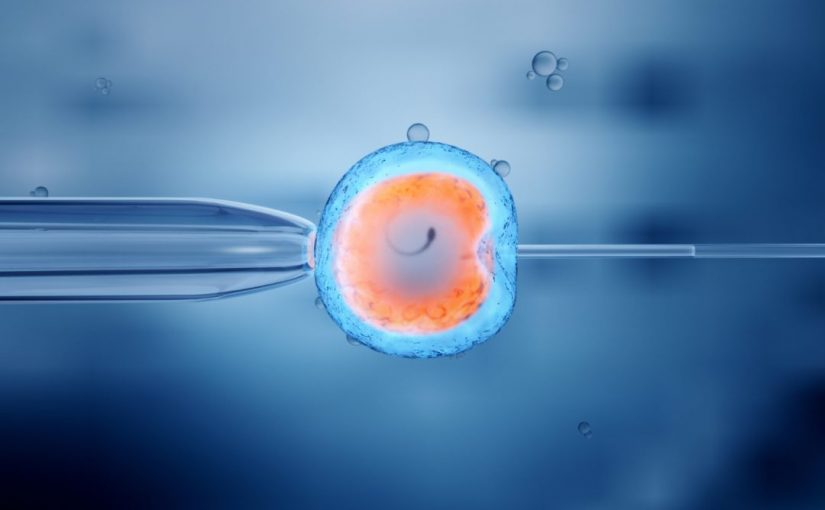
Assisted reproductive technologies – more generally referred to as in-vitro fertilisation or IVF – are increasingly common around the world. In fact, in Australia and New Zealand alone, more than 70,000 treatment cycles are performed each year.
What is important to know, is that pathology plays an integral role in IVF treatments. And the extent to which certain tests can help individuals and couples prepare for and support IVF treatments is constantly evolving.
Dr Melody Caramins, a genetic pathologist working at Laverty Pathology said;
“Pathology is actually one of the key components of all medical decisions but particularly in some settings more than others. IVF is definitely one of those settings where things are monitored very closely with pathology to ensure a healthy pregnancy.”
The pathology of IVF
The reasons for choosing IVF are many and varied. From physical factors such as age to genetic conditions, inherited disease or other factors, the use of IVF is commonplace.
However, before beginning IVF treatment, couples looking to conceive will undergo pathology testing to investigate any factors that may be affecting the fertility of either parent and to check they are healthy and able to begin the process.
Tests for women include blood tests looking at fertility hormones such as oestradiol, Luteinising Hormone, Follicle Stimulating Hormone (FSH), Anti-Mullerian Hormone (AMH) and progesterone.
These can indicate if the woman’s reproductive organs such as the ovaries are functioning properly.
Men will need to undergo sperm analysis which looks at sperm count, motility and morphology. This means looking at the number of sperm as well as their shape, size and movement. This is important to ensure enough healthy sperm is being produced.
Prospective parents will also need to be screened for STIs and diseases such as HIV and Hepatitis before beginning IVF.
Genetic pathology
Pathology is also opening new areas of understanding for potential parents, with improvements in genetic testing now more advanced, accessible and affordable than ever before.
Genetic testing can give parents an insight into pre-natal and post-natal health of their future child.
Carrier screening is a growing area of genetics that can test prospective parents for inherited conditions that could be passed on to their babies that have serious consequences and may even be fatal.
Genetic pathologists can now test parents’ DNA for disorders like Haemophilia, Cystic Fibrosis, Fragile X syndrome and Spinal Muscular Atrophy which are identifiable through blood tests.
How can genetic testing help?
As science advances so too does our understanding of the role of genetics in pregnancy and infertility as well as how genetic testing can be used to help parents make decisions before getting pregnant.
“Cystic fibrosis is a disease that many people are familiar with,” says Dr Caramins.
“What people don’t know is that you can have a mild form [of the disease], or a more severe form of the disease. And one of the mildest forms of cystic fibrosis affects sperm production, where the tubes that carry sperm out of the testes don’t develop properly” she says.
Genetic pathology techniques can be applied by embryologists to alert parents early on to issues that may influence the pregnancy’s success – this is known as pre-implantation genetic screening.
Dr Caramins also suggests genetic testing undertaken during IVF treatment can help people better understand their options.
“Women who use IVF often undergo a couple of cycles of treatment. The process costs money, and all pregnancies are precious, but these are more difficult pregnancies, so understandably there’s more anxiety around them,” she says.
What may be considered the most important pathology test for parents though is not a genetic test. The test anticipated with the most trepidation and excitement is the Beta HCG test, a blood test that confirms if a woman is pregnant.