Personalised medicine has revolutionised cancer care. Using pathology to test the genetic characteristics of a cancer, doctors can determine if a particular treatment will work, therefore reducing treatment times and increasing the likelihood of a positive outcome.
Recent research has made significant advances in the treatment of lung cancer thanks to the development of a new test to detect KRAS gene mutations.
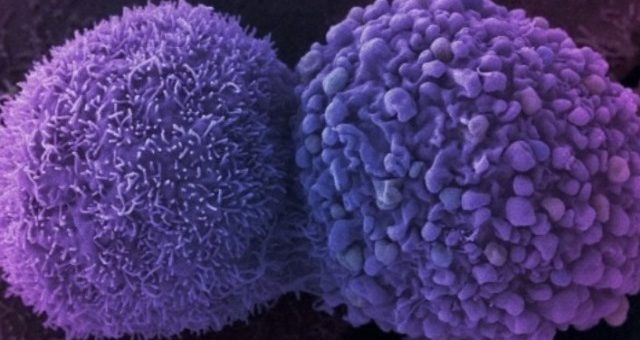
The KRAS gene produces proteins called K-Ras that influence when cells divide. Mutations in K-Ras can result in normal cells dividing uncontrollably and turning cancerous. Genetic mutations of KRAS occur in approximately 30% of lung cancer cases, and are associated with aggressive, chemo-resistant tumours with poor prognosis.
According to Cancer Council Australia lung cancer is the fifth most common cancer in Australia but the most common cause of cancer death, responsible for almost one in five cancer deaths in Australia.
Earlier this year researchers developed a “liquid biopsy” to detect KRAS mutation in patients with the most common form of lung cancer – non-small cell lung cancer – and initial trials have been promising.
A traditional lung biopsy involves removing tumour tissue via a needle biopsy or surgery under general anaesthetic.
A “liquid biopsy” involves taking a blood sample that can then be analysed to detect tumour DNA and look for particular mutations in the DNA. In the case of lung cancer, the blood sample can be analysed to look for the mutated KRAS gene and this can then inform doctors on the best treatment course.
Analysing genetic characteristics is already common practice for patients presenting with colorectal cancer (CRC) who will undergo KRAS testing to determine suitability for certain treatments.
The Economic Value of Pathology report released by Pathology Awareness Australia in April 2016 examined the benefits of this KRAS testing for colorectal cancer and the findings were significant. Between 1982 and 1986, 5–year survival was 47 per cent. Between 2007 and 2011, as KRAS testing became more common in CRC patients, this increased to 67 per cent, meaning patients have a 67 per cent chance of surviving for 5 years.
Initial findings from research into the role of KRAS mutations in lung cancer patients suggest that we could soon see a similar positive trend for them too.