Cancer treatment has made enormous progress in the last decade and continues to move forward at a rapid pace as scientists learn more about the disease.
As in many areas of medicine, genetics is driving the improvement in cancer care and pathology is integral to making new discoveries about the genetic characteristics of cancer. New pathology tests are also developed as part of keeping pace with advances in knowledge and treatment.
Bowel (or colorectal) cancer is the second biggest cancer killer in Australia.
One type of drug that is used to treat bowel cancer is known as an epidermal growth factor receptor (EGFR) inhibitor.
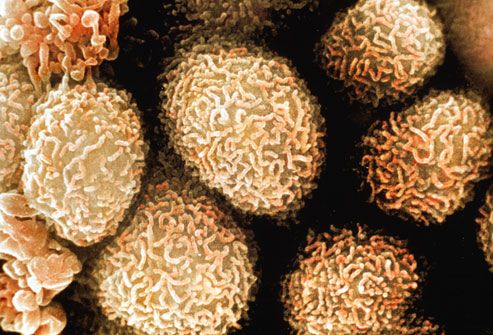
EGFRs are receptors that are present on the cell membrane. They receive chemical signals from outside the cell and have an important role in controlling normal cell growth. If a change happens within the receptor they can malfunction and cause unregulated cell division. This can be responsible for cancer growth.
The EGFR inhibitor drugs work by suppressing these malfunctioning receptors and therefore stalling progression of the cancer.
However, in some people the drugs do not work well and the cancer resists their effects and continues to grow. Research has shown that resistance can be predicted by pathology testing of the cancer to look for mutations in a group of genes known as RAS genes.
Tests are conducted on a biopsy of the cancer to look for certain mutations in these genes meaning that the cancer will not respond to the EGFR inhibitors.
This information can avoid prescribing drugs that will have little benefit and are expensive.
The test also saves time; allowing doctors to explore other treatment avenues for these patients more quickly.
The recently released Economic Value of Pathology report included evidence about the falling mortality rate for colorectal cancer and the benefits of RAS testing for patients and health spending:
“expanding testing to include all RAS mutations and limiting subsidy of cetuximab (an EGFR inhibitor) to those patients demonstrated to have no RAS mutations both reduces harms and improves health outcomes, and the cost of RAS mutation testing is negligible compared to the cost of therapy for patients with metastatic colorectal cancer”.
According to Bowel Cancer Australia, who are proud supporters of the Know Pathology Know Healthcare initiative, all advanced bowel cancer patients should undergo a RAS biomarker test to help determine their treatment options, minimise side effects, maximise survival rates and reduce toxicity exposure.
“Increased access to RAS testing will ensure the right treatment will be available at the right time for metastatic bowel cancer patients,” said Bowel Cancer Australia CEO, Julien Wiggins.
The current survival rate for bowel cancer is 67% and although this has risen by 20% in the last 30 years, the cancer still kills more than 4,000 Australians a year.
Bowel cancer screening programs rely on pathology, diagnosis is made by pathology and tests to guide treatment are conducted by pathology.
As medical research and the fight against cancer continue, pathology testing remains at the forefront saving time, money and ultimately, lives.